Your heart is the ultimate overachiever, beating roughly 100,000 times a day. When it starts sending SOS signals, it’s not just being dramatic—it’s asking for help.
In the world of cardiovascular medicine, every second counts. Common chest pain causes can range from a simple case of acid reflux to a life-threatening emergency. Knowing the difference between anxiety vs. heart attack symptoms is difficult for anyone to do at home, which is why modern diagnostic tools are so vital.
Whether you are experiencing shortness of breath (dyspnea) or heart racing symptoms like a fluttering chest, today’s technology allows doctors to see exactly what’s happening in real-time. Here are the essential tests that are redefining heart health in 2026.
-
The Front Line: EKG and Cardiac Biomarkers
When you arrive at a clinic with discomfort, the “gold standard” of care begins with two immediate tests to rule out a crisis.
The Electrocardiogram (EKG or ECG)
The EKG remains the most critical initial tool. It records the heart’s electrical activity and can identify a major heart attack within minutes. Current 2025–2026 guidelines emphasize that an EKG should be performed and interpreted within 10 minutes of arrival.
- Why it matters: Beyond detecting heart attacks, it is the primary way to diagnose irregular rhythms that could lead to sudden cardiac arrest.
High-Sensitivity Troponin (hs-cTn)
Think of Troponin as a “chemical flare” sent out by the heart. When heart muscle is damaged, these proteins are released into the blood. Modern high-sensitivity assays (hs-cTn) allow doctors to detect even tiny amounts of injury much earlier than older tests. New “0/1-hour” protocols mean doctors can confirm or rule out a heart attack in a fraction of the time it used to take.
-
Deep Dives: EKG vs. Echocardiogram and Stress Tests
If your initial EKG is clear but you still feel “off,” doctors look at the heart’s structure and how it handles work.
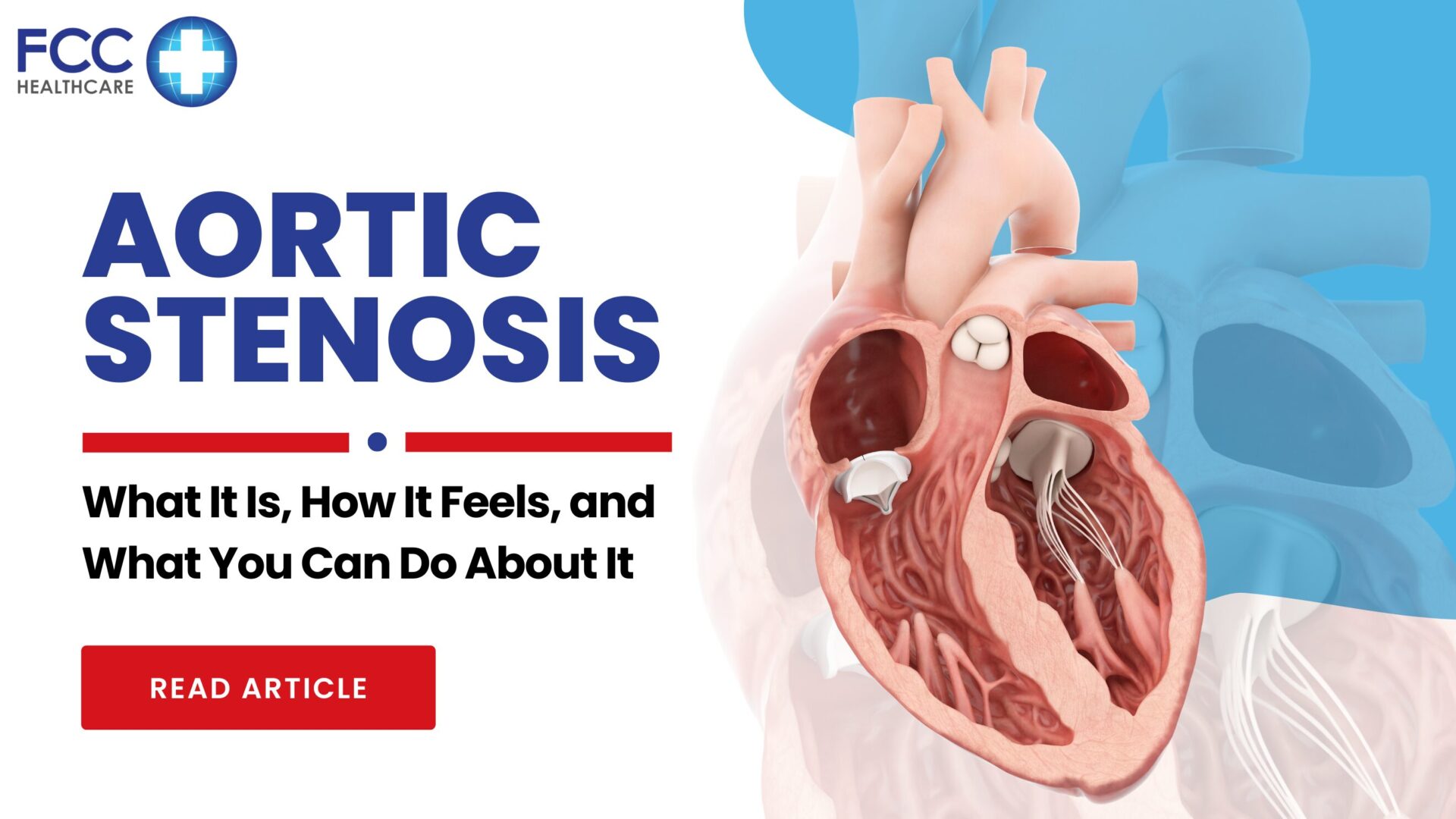
Transthoracic Echocardiogram (TTE)
Many patients wonder about the difference between an EKG vs. Echocardiogram. While the EKG looks at the heart’s electricity, the echocardiogram (a heart ultrasound) looks at its plumbing and structure. Echocardiogram can be used to assess conditions like –
- Heart Failure: It measures the “ejection fraction” (the heart’s pumping power).
- Valve Disease: It spots leaks or narrowing in the heart’s valves.
- Fluid: It detects dangerous fluid buildup around the heart.
Stress Test for the Heart
A stress test for the heart evaluates how your “engine” performs under pressure. You might walk on a treadmill or take a medication that simulates exercise. In 2026, stress imaging (using ultrasound or nuclear scans during the test) is the preferred method, as it shows exactly which parts of the heart aren’t getting enough blood during activity.
-
Advanced Imaging: The “Game-Changer” Non-Invasive Scan
One of the most significant shifts in cardiology is the rise of CT Coronary Angiography (CCTA).
In the past, checking for blockages required a “heart cath”—an invasive procedure using a catheter. Today, non-invasive heart imaging like the CCTA uses high-speed X-rays to create a 3D map of your arteries.
- Rule-Out Power: It has a nearly 100% “negative predictive value,” meaning if the scan is clear, you can go home with peace of mind.
- Early Detection: It can find “soft plaque” before it hardens, allowing for early intervention. This is often paired with a cardiac calcium score to assess your long-term risk of heart disease.
How These Pathways Save Lives
The real magic isn’t just in one test; it’s in the “diagnostic pathway.” By combining these tools, medical teams can:
- Catch “Silent” Attacks: Especially important for signs of heart attack in women, which can be subtle or atypical.
- Speed Up Treatment: Faster “door-to-balloon” times mean less heart muscle is lost during a blockage.
- Avoid Unnecessary Procedures: Non-invasive scans prevent patients from undergoing invasive procedures they don’t actually need.
- Identify Microvascular Disease: For those with persistent pain but “clear” major arteries, 2025 guidelines now help diagnose issues in the smallest blood vessels.
Conclusion
Chest pain, shortness of breath, and palpitations are more than just discomforts; they are windows of opportunity. In the landscape of 2026 cardiology, we no longer have to wonder if a symptom is serious. We have the best heart tests for early detection to know for sure and act fast.
If you or a loved one experiences these symptoms, don’t wait. Knowing when to see a cardiologist for palpitations or chest pain is the first step toward a longer, healthier life.